.webp)
Navigating the Evolving Medicare Advantage Landscape in Home Health and Hospice Care

Navigating the Evolving Medicare Advantage Landscape in Home Health and Hospice Care
The healthcare industry is experiencing a significant shift in the Medicare landscape, particularly in home health and hospice care. As revenue cycle management experts, we at RapidClaims understand the importance of staying ahead of these changes to ensure optimal financial health for healthcare providers. In this comprehensive guide, we'll explore the expanding Medicare Advantage (MA) landscape and provide strategies for managing the associated challenges.
The Growing Medicare Advantage Market
Recent data shows a remarkable growth in Medicare Advantage enrollment:
- In 2022, over 28 million beneficiaries enrolled in MA plans, representing nearly 48% of the eligible population.
- This marks an 8% increase from 2021, with 2.2 million new enrollees.
- For 2023, projections indicate 52 participating MA plans, totaling 9.3 million enrollees.
- MA plans now account for 26% of home health agency revenue and 28% of visits performed.
These statistics underscore the critical need for home health and hospice agencies to adapt to the changing payer mix and prepare for the challenges and opportunities that come with increased MA participation.
Impact on Home Health and Hospice Agencies
The expansion of Medicare Advantage plans brings several implications for providers:
1. Shifting Payer Mix: Agencies must prepare for a higher proportion of MA patients in their overall patient load.
2. Authorization Requirements: MA plans often have stringent authorization processes, necessitating thorough research and preparation.
3. Increased Claim Denials: With more MA patients, agencies may face a higher volume of claim denials due to various factors such as inaccurate information or missed authorization deadlines.
4. Potential for Lower Reimbursements: MA plans may offer lower reimbursement rates compared to traditional Medicare, impacting agency revenues.
5. Inconsistent Adoption of Medicare Regulations: Some MA plans may not follow traditional Medicare regulations, such as the Patient-Driven Groupings Model (PDGM) or Notice of Admission (NOA) requirements.
6. Telehealth Expansion: Agencies need to understand the billing requirements and service charges associated with telehealth services under MA plans.
7. Value-Based Purchasing: The future of healthcare is moving towards value-based models, and agencies must be prepared to demonstrate their value proposition.
Strategies for Managing Medicare Advantage Plans
To effectively navigate the MA landscape, agencies should consider the following strategies:
1. Learn Common Requirements and Challenges
- Understand the nuances of eligibility verification for MA plans.
- Familiarize yourself with authorization processes, including initial and ongoing requirements.
- Be aware of potential longer claim processing times and variances in billing codes.
- Prepare for more complex appeals processes that may require extensive documentation.
2. Research Plans Thoroughly
- Identify covered benefits and services for each MA plan.
- Understand authorization requirements and processes.
- Determine if medical record reviews are needed and what collaboration the plan expects.
- Research timely filing guidelines and payment timelines.
- Understand payment options (per visit, per hour, or episodic).
3. Negotiate Effectively
- Come prepared with data analytics showcasing your agency's performance.
- Understand your costs and margins to negotiate fair rates.
- Be ready to discuss quality outcomes, rehospitalization rates, and patient satisfaction scores.
4. Build a Strong Value Proposition
- Use data to demonstrate your agency's value to payers.
- Highlight quality outcomes, patient satisfaction, and cost-effectiveness.
- Show how your agency can help MA plans achieve their goals of improving care quality while controlling costs.
5. Understand the VBID Model for Hospice
- Familiarize yourself with the Value-Based Insurance Design (VBID) model for hospice care.
- Stay informed about the evolving landscape of VBID and its impact on hospice services.
6. Implement Robust AR Management Practices
- Track and measure unbilled AR regularly.
- Aim for unbilled AR to be less than 10% of average monthly revenue for AR over 30 days.
- Monitor outstanding orders and clinical documentation timeliness.
- Implement pre-bill audit processes to reduce billing delays.
7. Develop Key Performance Indicators (KPIs)
- Track metrics such as days to Notice of Admission (NOA) or Notice of Election (NOE), days to bill, AR over 90 days, and collections to revenue ratio.
- Use these KPIs to identify areas for improvement and optimize your revenue cycle.
Leveraging Technology for Success
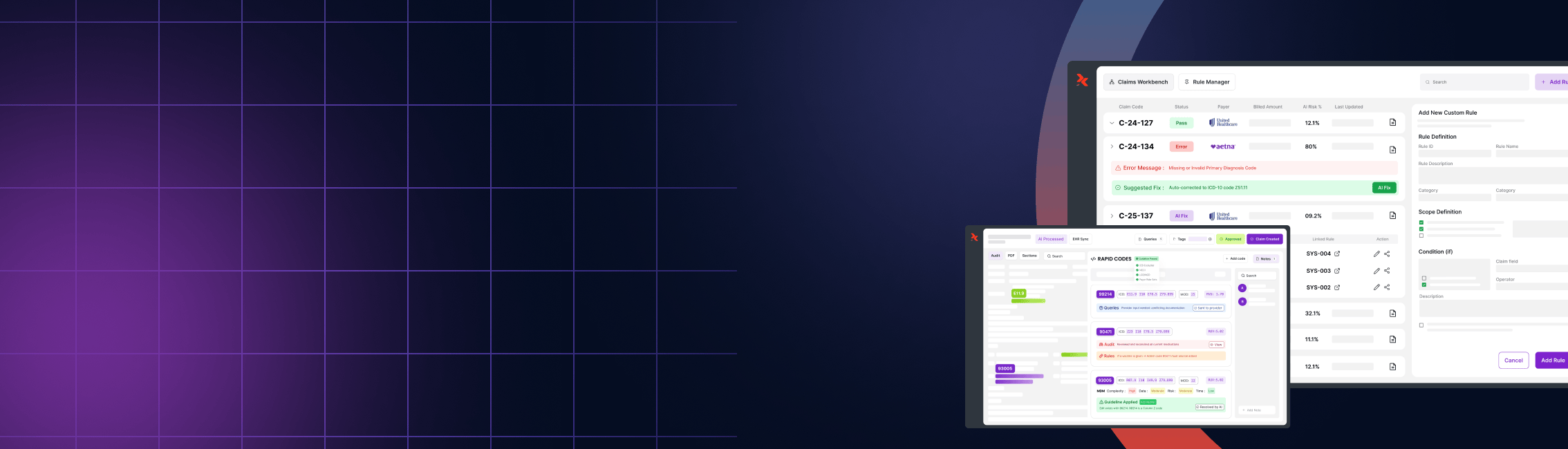
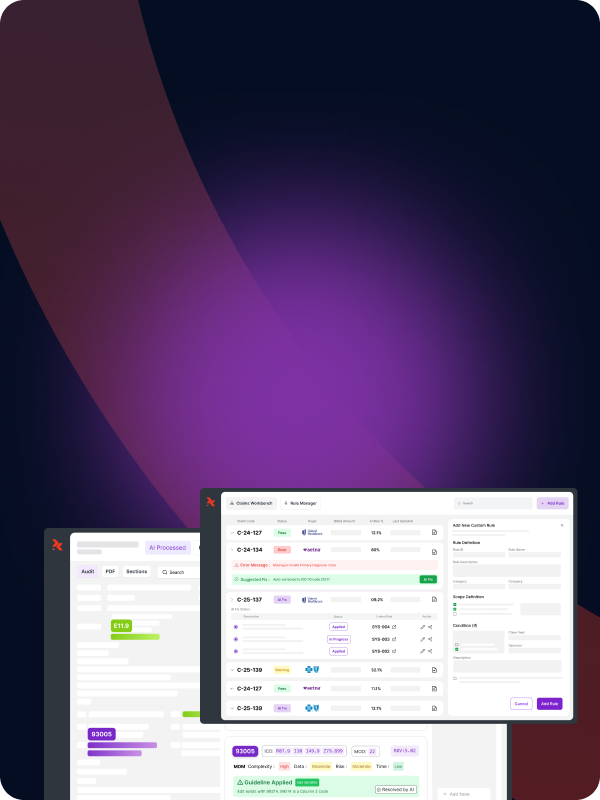
At RapidClaims, we understand the complexities of managing revenue cycles in the evolving Medicare Advantage landscape. Our AI-powered coding solution can help streamline your coding process, ensuring accuracy and compliance with the latest standards. By automating routine tasks, we enable your team to focus on more strategic aspects of MA plan management, such as payer negotiations and value proposition development.
Conclusion
The expansion of Medicare Advantage plans presents both challenges and opportunities for home health and hospice agencies. By understanding the landscape, implementing effective strategies, and leveraging advanced technologies like RapidClaims, agencies can navigate these changes successfully. Remember, the key to thriving in this new environment lies in proactive planning, data-driven decision-making, and a commitment to delivering high-quality, cost-effective care.
Stay ahead of the curve in revenue cycle management by partnering with RapidClaims. Our innovative solutions can help you optimize your processes, enhance accuracy, and improve your bottom line in the face of evolving Medicare Advantage challenges.
%201.png)