.webp)
Revolutionizing Healthcare Administration using Generative AI and Large Language Models

Understanding Generative AI and LLMs
Generative AI encompasses a broad range of models designed to produce content, such as text, music, or art. Among these, Large Language Models (LLMs) like ChatGPT, GPT-4, and BERT have garnered significant attention for their ability to process and generate human-like text based on given prompts.
LLMs are built on transformer architecture, which uses self-attention mechanisms to process input sequences. These models are trained on vast amounts of text data, often comprising hundreds of billions of tokens. By predicting the next word in a sequence, these models can generate coherent and contextually relevant responses.
The training process involves:
1. Pre-training: The model learns general language understanding from a diverse corpus of text.
2. Fine-tuning: The model is further trained on domain-specific data to improve performance on particular tasks.
LLMs operate on the principle of "few-shot learning," allowing them to perform tasks with minimal examples. This capability makes them particularly valuable for tasks involving text summarization, content creation, translation, and more.
Applications of LLMs in Healthcare RCM
The integration of LLMs in healthcare Revenue Cycle Management (RCM) presents numerous opportunities:
1. Patient Communication:
- LLMs can help rephrase complex medical concepts and benefits, making them more accessible to patients.
- This includes translating explanation of benefits (EOB) documents or providing clear answers through chatbots.
- Example: An LLM could take a technical EOB and produce a plain-language summary, explaining covered services, out-of-pocket costs, and next steps for the patient.
- LLMs can also generate personalized appointment reminders, reducing no-show rates and improving patient engagement.
2. Document Management:
- Specialists often handle a multitude of documents, including referral forms, insurance paperwork, and clinical notes.
- LLMs can automate document classification by understanding the content and context of each document.
- Key information extraction can be performed, pulling out relevant data points like patient demographics, diagnosis codes, and treatment plans.
- Example: An LLM could process a batch of incoming documents, categorizing them into referrals, test results, and insurance claims, while extracting key information into a structured format for easy integration into electronic health records (EHRs).
3. Prior Authorization:
- Although still evolving, LLMs hold potential in determining medical necessity by analyzing patient history, clinical notes, and payer guidelines.
- LLMs can assist in compiling the necessary documentation for prior authorization requests.
- They can also help interpret complex payer policies and guidelines, suggesting the most appropriate codes and documentation to support the authorization request.
- Example: An LLM could review a patient's medical history, current symptoms, and proposed treatment plan, then generate a draft prior authorization request that includes all relevant clinical justifications and meets payer-specific requirements.
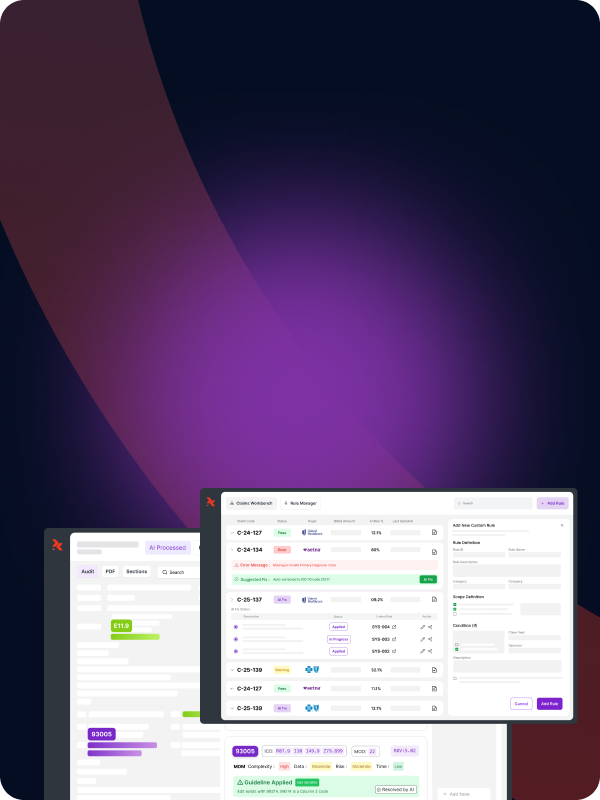
4. Denial Management:
- LLMs can be employed to generate structured denial reasons from payer letters and even create denial appeal letters based on specialists' notes.
- They can analyze historical denial patterns and suggest proactive measures to prevent future denials.
- LLMs can assist in prioritizing denials based on the likelihood of successful appeal and potential financial impact.
- Example: An LLM could analyze a denial letter, extract the specific reason for denial, and automatically generate an appeal letter that addresses the payer's concerns, citing relevant clinical guidelines and patient-specific information.
5. Coding Assistance:
- LLMs can assist coders by suggesting appropriate ICD-10 and CPT codes based on clinical documentation.
- They can help in identifying missing or incomplete documentation that may lead to downcoding or claim denials.
- Example: An LLM could review a physician's notes from a patient encounter and suggest the most appropriate diagnosis and procedure codes, flagging any areas where additional documentation might be needed to support a higher-level code.
6. Revenue Forecasting and Analysis:
- By analyzing historical claim data, payer contracts, and current patient demographics, LLMs can assist in predicting future revenue streams.
- They can identify trends in reimbursement patterns and suggest areas for improvement in the revenue cycle.
- Example: An LLM could analyze the past year's claims data, current payer mix, and upcoming contract changes to forecast expected revenue for the next quarter, highlighting any potential areas of concern or opportunity.
Challenges and Considerations
While the potential of LLMs in healthcare is vast, several challenges must be addressed:
Privacy and Compliance:
- Ensuring patient health information (PHI) security is paramount.
- HIPAA compliance is crucial when implementing LLMs in healthcare settings.
- Data anonymization techniques must be employed when training or fine-tuning models on patient data.
- Example: Implementing federated learning approaches where the model is trained across decentralized devices holding local data samples, without exchanging them.
Accuracy and Hallucinations:
- LLMs can sometimes produce plausible but incorrect information, known as hallucinations.
- Continuous validation and fine-tuning are essential to maintain accuracy.
- Implementing human-in-the-loop systems where AI-generated content is reviewed by domain experts before being acted upon.
- Example: Using a confidence scoring system where the LLM's outputs are flagged for human review if they fall below a certain threshold.
Cost and Complexity:
- The computational resources required for training and running LLMs can be substantial.
- Evaluating the cost-benefit ratio and exploring simpler solutions where applicable is crucial.
- Consideration of edge computing solutions to reduce latency and data transfer costs.
- Example: Implementing a tiered approach where simpler, rule-based systems handle routine tasks, and LLMs are reserved for more complex, nuanced scenarios.
Bias and Fairness:
- LLMs can perpetuate or amplify biases present in their training data.
- Regular audits for bias in model outputs, especially in healthcare where equitable treatment is crucial.
- Example: Implementing fairness constraints in the model training process and regularly testing the model's performance across different demographic groups.
Interpretability and Explainability:
- The "black box" nature of LLMs can be problematic in healthcare, where understanding the rationale behind decisions is crucial.
- Developing methods to provide clear explanations for model outputs, especially for clinical decision support applications.
- Example: Implementing attention visualization techniques to highlight which parts of the input text most influenced the model's output.
The Future of LLMs in Healthcare
As LLM technology continues to evolve, its applications in healthcare RCM will expand. Future developments may include:
1. Multimodal Models: Integration of text, image, and potentially audio data for more comprehensive analysis. For example, an LLM could analyze both clinical notes and medical imaging reports to assist in coding and prior authorization.
2. Improved Domain Specificity: More sophisticated fine-tuning techniques will allow for better performance on healthcare-specific tasks without compromising general language understanding.
3. Enhanced Privacy-Preserving Techniques: Advancements in federated learning and differential privacy will make it easier to train models on sensitive healthcare data without compromising patient privacy.
4. Real-time Learning and Adaptation: Future LLMs may be able to continuously learn and adapt to new information, such as updated billing codes or payer policies, without requiring full retraining.
5. Integration with Robotic Process Automation (RPA): Combining LLMs with RPA could automate end-to-end processes in the revenue cycle, from initial patient registration to final payment posting.
Conclusion
The integration of Generative AI and LLMs in healthcare administration promises to transform how tasks are handled, bringing about increased efficiency and accuracy. However, careful consideration of privacy, compliance, accuracy, and cost is essential to fully harness the potential of these technologies.
As we look to the future, continuous innovation and mindful implementation will be key to revolutionizing healthcare administration through AI. Healthcare organizations that successfully navigate these challenges and leverage the power of LLMs stand to gain significant advantages in operational efficiency, patient satisfaction, and financial performance.
%201.png)