.webp)
Coding for Telehealth and Telemedicine Services


As telehealth continues to shape the healthcare industry, coding and billing for these services have become increasingly complex. Initially, telemedicine was a niche offering primarily used in rural areas.
However, the COVID-19 pandemic accelerated its adoption, making it a vital component of healthcare delivery worldwide. For healthcare providers, staying up-to-date with the correct telehealth CPT codes and modifiers is essential to ensure accurate billing and timely reimbursement.
Accurate telehealth coding ensures compliance and helps providers avoid costly billing errors and service delays. Missteps in the coding process can lead to claim denials, underpayment, or even legal issues, making it critical for healthcare professionals to understand the nuances of telemedicine billing practices.
This article will break down the various telehealth coding aspects, including the changes post-COVID-19, place of service (POS) codes, and essential modifiers.
Importance of Accurate Billing for Telemedicine Services
When telemedicine emerged as a solution to improve patient access to care during the pandemic, the coding system quickly adapted to the new reality. Telehealth coding, however, involves unique complexities. The main difference between telemedicine and in-person care coding lies in the Place of Service (POS) codes, the addition of modifiers, and the need for understanding payer policies.
Properly selecting the right CPT codes and modifiers ensures that telemedicine services are reimbursed accurately, which directly impacts the financial health of your practice or organization. For example, using the wrong POS code or failing to apply the correct modifier can lead to claims being denied or underpaid. As healthcare continues to evolve, understanding these technicalities is becoming even more essential, especially with the changes coming in 2025.
As the industry moves away from the flexibility introduced by the COVID-19 public health emergency (PHE), payers (including Medicare, Medicaid, and private insurers) are returning to stricter policies. To stay compliant, healthcare organizations must understand the evolving coding rules for telehealth services. Using tools like Rapidclaims.ai can be a game-changer in ensuring you're up to speed with the latest changes.
Telehealth Policies and Their Evolution Post-COVID-19
The policies surrounding telehealth coding have evolved significantly since the COVID-19 pandemic. Initially, many restrictions around telehealth CPT codes were loosened to provide better access to care.
This included expanding the range of services covered by telehealth and allowing more flexibility around patient locations and the use of non-HIPAA-compliant technologies.
However, as we move into 2025, healthcare providers will once again face tighter restrictions. Medicare and other payers are gradually transitioning to pre-pandemic policies, which means telehealth CPT codes may no longer cover all services, and certain restrictions on geographic location or patient site of care will be reinstated.
To keep up, healthcare providers must be proactive in reviewing the latest telehealth CPT codes and understanding how their use has changed. If you're relying on outdated codes or don’t adjust to payer requirements, you may see delays or denials in reimbursement.
Coding for Common Telehealth Visits
As telehealth has become a more integral part of healthcare delivery, accurate coding for telemedicine services is critical. Whether it's a video consultation or an audio-only check-in, knowing the correct telehealth CPT codes to use will ensure that your services are properly reimbursed.
Coding for Audio-Video Telehealth Services
Telehealth services are not limited to voice-only communications. As healthcare continues to embrace digital solutions, audio-video telehealth services have become the standard for many providers.
Using the correct telehealth CPT codes for these services is essential for maximizing reimbursement and ensuring compliance with payer policies.
1. Standard CPT Codes for Telehealth: 99202-99215
For audio-video telehealth visits, healthcare providers should use the standard CPT codes for office visits, 99202-99215. These codes are used to report evaluation and management (E/M) services, whether the visit takes place in-person or via telehealth. The primary difference when using telehealth CPT codes is the Place of Service (POS) and sometimes the addition of a modifier to indicate the use of telemedicine.
The 99202-99215 codes vary based on the complexity of the visit and the level of service provided. For example:
- 99202-99205: For new patients, ranging from straightforward to more complex visits.
- 99211-99215: For established patients, also covering a range from low to high complexity.
The key is ensuring that the telehealth CPT codes reflect the appropriate complexity of the visit, just as if it were an in-person encounter. Additionally, the visit’s duration and medical decision-making (MDM) are crucial factors when determining the appropriate code.
2. Place of Service Codes: POS 02 and POS 10
As mentioned earlier, POS codes are essential when billing for telehealth services. The two most common POS codes used for telehealth visits are:
- POS 02: Used when the telehealth service is provided from a location other than the patient’s home, such as a clinic or hospital.
- POS 10: Used when the patient receives telehealth services in their home.
These codes are significant because they help determine the reimbursement rate. POS 10 services, provided at the patient’s home, tend to be reimbursed at a higher rate than those delivered through POS 02.
As we move into 2025, it’s important to check with payers to see if there will be any changes to POS codes or reimbursement rates based on the site of service. As telehealth becomes more common, the use of these codes will play a significant role in the billing process.
3. Payment Distinctions and the Need for Policy Reviews with Medicare and Private Payers
Different payers handle payment for telehealth services in different ways. For example, Medicare has specific policies that may differentiate between telehealth services provided at a clinic (POS 02) and those provided in the patient’s home (POS 10).
With the upcoming policy changes in 2025, Medicare will begin restricting certain telehealth services to patients in rural areas or health professional shortage areas (HPSAs).
This makes it essential for healthcare providers to stay up-to-date on the evolving policies of Medicare and private payers. Regularly reviewing payer policies and confirming coverage for telehealth services is critical for ensuring that the correct telehealth CPT codes are used and reimbursement is accurate.
Coding for Audio-Only Visits
Audio-only visits, which allow patients to communicate with providers via phone, have become increasingly common, especially for patients who don't have access to video technology. Let's look at how to code for these services.
1. Medicare Discontinuation of Certain CPT Codes Post-January 2025
Currently, Medicare reimburses for a range of audio-only telehealth CPT codes, such as 99441-99443. However, starting January 2025, these codes will be discontinued. Instead, Medicare will allow audio-only communication for services related to mental health or substance use disorders, but these visits will be limited to specific circumstances.
This change underscores the importance of keeping up-to-date with the latest telehealth CPT codes and understanding how services like audio-only visits will be reimbursed. Providers will need to prepare for the shift in policy and ensure they are using the right codes before January 2025.
2. Importance of CPT Modifier 93 for Audio-Only Services
When coding for audio-only visits, it's important to use the appropriate CPT modifier to indicate that the service was provided via an audio-only system. Modifier 93 is used to identify these services and should be added to the appropriate CPT codes.
For instance, if you're billing for an audio-only evaluation and management service, you would append modifier 93 to CPT codes 99441-99443 (until 2025) or the new audio-only codes. This ensures that the service is recognized as telehealth and reimbursed accordingly.
3. Guidelines for Audio-Only Services Across Different State and Provider Policies
Since state and provider policies vary, it’s crucial to check with each payer to understand the requirements for audio-only telehealth services. While Medicare has specific guidelines, private payers may have different rules, especially regarding the use of telehealth CPT codes and modifiers.
For example, some states may allow audio-only visits for a broader range of services, while others may limit them to specific healthcare fields, like mental health or primary care. Always check your local policies to stay compliant.
Virtual and Digital Visit Coding
Telehealth and telemedicine services continue to evolve, and coding requirements for these services are becoming increasingly specific and varied. As healthcare providers adapt to virtual and digital consultations, it's essential to stay informed about the correct coding practices to ensure reimbursement and compliance.
1. E-Visit CPT Codes
The CPT codes for e-visits are essential for documenting and reimbursing digital consultations. These codes are used for patient-initiated online communications with healthcare providers, typically for non-urgent matters.
Updated E-Visit CPT Codes (2025):
The American Medical Association (AMA) has introduced new codes to replace the previous e-visit codes (CPT 99421–99423). These include:
- CPT 98000: Online evaluations lasting 5–10 minutes.
- CPT 98001: Online evaluations lasting 11–20 minutes.
- CPT 98002: Online evaluations lasting 21 minutes or more.
These codes reflect the time spent on virtual consultations and require proper documentation to justify the time spent with each patient. Always ensure that the encounter is patient-initiated and meets the criteria outlined by AMA guidelines.
3. HCPCS Codes for Virtual Check-Ins
HCPCS codes are used for various telehealth-related services, especially virtual check-ins.
Updated HCPCS Codes (2025):
Some HCPCS codes have been replaced with new CPT codes for better alignment with telehealth practices:
- G2010: Used for remote evaluation of recorded video or images submitted by a patient (unchanged).
- CPT 98016: Replaces G2012 for brief synchronous communication technology-based services, typically lasting 5–10 minutes.
- G2252: Used for extended virtual check-in services (unchanged).
These codes are critical for documenting brief virtual interactions initiated by patients.
4. Clarification on POS or Modifier Requirements
Place of Service (POS) codes and modifiers play a vital role in accurately documenting virtual and digital visits. The appropriate modifier should be applied based on whether the visit occurred via live, interactive video or audio-only communication.
- Modifier 95: Indicates that the service was provided via telecommunication technology (live video).
- Modifier FQ: Indicates audio-only telehealth services, which became widely recognized during the pandemic and remain valid in 2025.
Healthcare providers must ensure they use the correct POS code to reflect where the service was provided (e.g., POS 02 for telehealth provided in a location other than the patient’s home).
Comparison of Audio-Video, Audio-Only, and Virtual-Digital Telehealth Visits
Telehealth services have evolved into multiple formats, each with distinct features and billing requirements. To better understand how they differ, here’s a detailed comparison of Audio-Video Telehealth Visits, Audio-Only Visits, and Virtual-Digital Visits (E-Visits).
This table highlights the main distinctions in communication types, billing codes, and the scope of services provided, allowing healthcare providers to easily navigate the complexities of telemedicine coding.
Limitations Based on Geographic and Originating Site Requirements
A key element to consider when coding for telehealth visits is the Place of Service (POS) code. As telehealth evolved during the pandemic, many restrictions were lifted to allow patients to receive care from home. However, with changes in 2025, telehealth CPT codes will again be restricted based on the patient’s geographic location.
For example, POS 02 (Telehealth Provided Other than in a Patient’s Home) will be used when the patient is at a facility or other location, while POS 10 (Telehealth Provided in a Patient’s Home) will be applicable when the patient is at home. These distinctions play a significant role in determining the correct reimbursement rates.
Many private payers have already started to enforce similar restrictions, so it’s crucial to understand how telehealth CPT codes need to be applied, depending on where the service is provided.
Telemedicine CPT and HCPCS Codes

When it comes to telemedicine coding, proper use of CPT and HCPCS codes ensures that healthcare providers receive reimbursement for remote services. These codes reflect various types of consultations, from in-depth evaluations to simple check-ins.
1. Commonly Used Telemedicine CPT Codes
For telemedicine visits, many CPT codes mirror those used for in-person consultations but require modifiers to indicate they were conducted virtually.
- CPT 99202–99215: Evaluation and management (E/M) services based on complexity and time spent during the consultation.
- CPT 99341–99350: Home visits conducted via telehealth for established patients.
2. HCPCS Codes for Telehealth Services
HCPCS codes play an integral part in telehealth services and are used for various telecommunication-based visits. As mentioned above, codes like G2010, G2012, and G2252 are designed to classify virtual check-ins and digital health services.
3. Use of Modifiers and Importance of Reviewing Policy Requirements
Modifiers such as 95 (telecommunication technology) or FQ (audio-only) are essential for indicating how services were delivered. Healthcare providers should review insurance policies regularly to understand specific guidelines regarding code usage, modifiers, and coverage criteria.
Preventing Common Telehealth Billing Mistakes

Accurate billing is critical in telehealth, but errors can lead to denials or delayed reimbursements. Here are some tips to avoid common mistakes:
1. Keeping Up with Correct Billing Codes for Telehealth
Telehealth codes are updated regularly by organizations like AMA and CMS. Staying informed about these updates ensures your practice uses the correct codes.
2. Ensuring Proper Post-Visit Documentation for Reimbursement
Proper documentation is crucial after a telehealth visit. Include accurate notes detailing the consultation, patient consent for telehealth services, time spent during the visit, and a summary of care provided.
3. Training Teams on Telehealth Billing Processes
Telehealth billing can be complex, so regular training is key to minimizing errors. Ensure your billing team is familiar with current guidelines, including code usage, modifiers, and payer-specific policies.
4. Verifying Service Coverage with Patient’s Insurance
Before performing any telehealth service, verify coverage with the patient’s insurance provider. This prevents denials and ensures both provider and patient understand what is covered under their plan.
Conclusion
Proper coding for telehealth and telemedicine services is crucial to ensure accurate reimbursement, compliance, and smooth operation in an increasingly digital healthcare environment.
As telemedicine evolves, staying updated on the latest telehealth CPT codes, modifiers, and payer policies is essential to avoid costly billing errors and claim denials. Understanding the nuances of Place of Service (POS) codes, audio-only visits, and virtual check-ins will help healthcare providers optimize reimbursement and remain compliant.
As regulations continue to shift, particularly with upcoming policy changes in 2025, it's essential for healthcare professionals to adapt and maintain accurate coding practices to ensure continued success in telehealth billing.
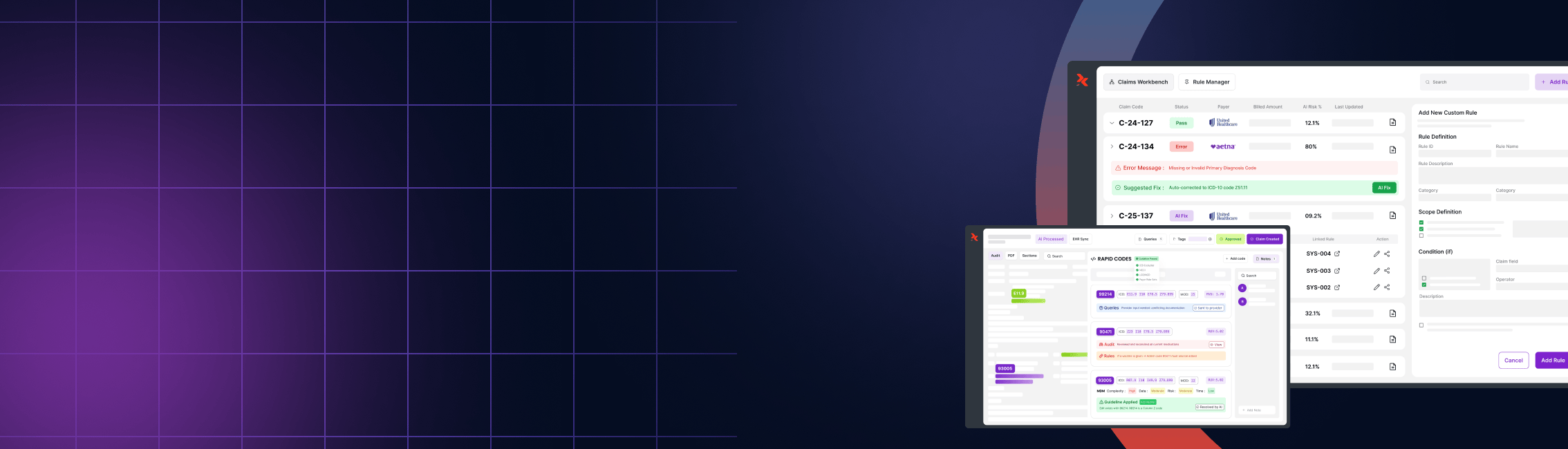
Simplify Telehealth Billing with Rapidclaims.ai
Navigating the complexities of telehealth coding and billing can be overwhelming, especially as telemedicine continues to evolve. With the ever-changing telehealth CPT codes and payer policies, it’s critical to stay up-to-date to avoid billing errors and claim denials.
Rapidclaims.ai offers an intelligent solution to streamline your telehealth billing process. Our AI-powered platform ensures you’re using the correct codes, modifiers, and Place of Service (POS) codes every time, minimizing the risk of errors and maximizing reimbursement. With Rapidclaims.ai, you can:
- Stay up-to-date with the latest changes to telehealth CPT and HCPCS codes, including adjustments for 2025.
- Automate code selection based on the type of service (audio-video, audio-only, virtual check-ins, etc.).
- Ensure accurate modifiers like modifier 95 for telemedicine or modifier FQ for audio-only services.
- Easily manage documentation and billing submissions to streamline your entire telehealth workflow.
Don’t let coding complexities slow down your practice's financial health. Rapidclaims.ai helps you stay compliant, reduce billing errors, and improve your reimbursement process—all while saving valuable time.
Try Rapidclaims.ai today and simplify your telehealth billing with confidence!
Frequently Asked Questions (FAQ)
1. How do modifiers work in telehealth coding?
In telemedicine billing, modifier -95 is used for synchronous audio/video visits, while modifier GT applies to interactive audio/video services. POS 02 is used for telehealth outside the patient’s home, and POS 10 is for telehealth provided at the patient’s home. These modifiers and POS codes ensure accurate billing and compliance.
2. What is the significance of Place of Service (POS) codes for telehealth?
Place of Service (POS) codes are crucial for telehealth billing as they reflect the location where the service was provided. Common POS codes include POS 02, used for telehealth provided in settings other than a patient’s home, and POS 10, which is used when the service is provided in the patient’s home. These codes directly affect reimbursement rates and are essential for accurate billing.
3. Are there specific telehealth CPT codes for audio-only visits?
Yes, CPT codes for audio-only telehealth visits are used for consultations that take place over the phone without the use of video. In 2025, Medicare will discontinue certain audio-only codes, so it’s important to keep up with changes. CPT modifier 93 is applied to audio-only visits to identify them as telehealth services.
4. How do telehealth policies differ post-COVID-19?
The telehealth policies that were relaxed during the COVID-19 pandemic are now tightening as healthcare systems move towards pre-pandemic regulations. This includes stricter POS codes and geographic location restrictions for telehealth services. It’s important for healthcare providers to stay updated on these policy changes to avoid billing errors and ensure compliance.
5. How can Rapidclaims.ai help with telehealth coding?
Rapidclaims.ai simplifies the process of telehealth coding by providing AI-powered tools to automate code selection, track the latest updates to telehealth CPT codes, and ensure the proper use of modifiers and POS codes. This reduces billing errors, improves reimbursement accuracy, and helps healthcare providers stay compliant with changing regulations.
6. What changes in telehealth coding should healthcare providers prepare for in 2025?
In 2025, healthcare providers should be aware of the return to stricter telehealth coding policies, including limitations on audio-only services and stricter POS code guidelines. As payers, including Medicare, shift back to pre-pandemic regulations, it’s essential to adjust coding practices and keep up with payer-specific requirements to avoid claim denials.
%201.png)