.webp)
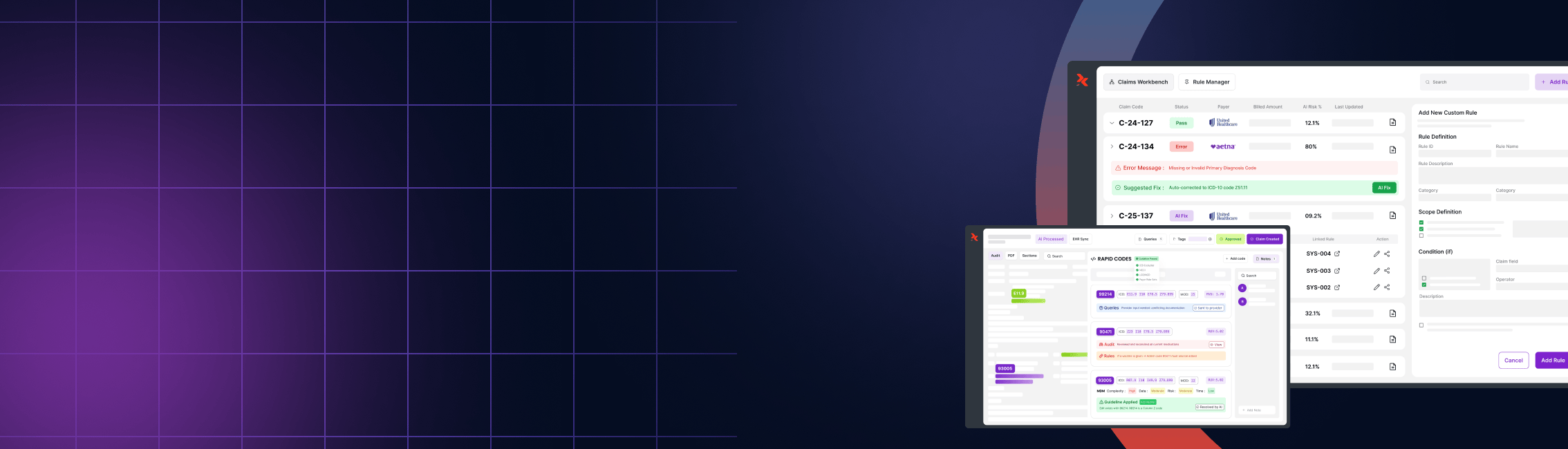
Unleashing the Power of AI in Medical Coding: Revolutionizing Revenue Cycle Management

Unleashing the Power of AI in Medical Coding: Revolutionizing Revenue Cycle Management
The healthcare industry is undergoing a significant transformation, driven by the integration of advanced technologies. Among these, artificial intelligence (AI) is emerging as a game-changer, particularly in the realms of medical coding and revenue cycle management (RCM). The ability to process vast amounts of clinical documentation quickly and accurately is revolutionizing the way healthcare providers manage their billing and coding operations. In this blog, we delve into the impact of AI on medical coding, exploring how it enhances efficiency, accuracy, and compliance while driving cost savings and scalability for healthcare organizations.
The Role of AI in Medical Coding
Medical coding is a critical component of the healthcare revenue cycle, converting clinical documentation into standardized codes used for billing and insurance purposes. Traditionally, this process has been labor-intensive and prone to errors, often leading to delays in reimbursement and financial losses. However, the advent of AI in coding is changing the landscape, offering solutions that streamline the coding process, reduce human error, and improve overall efficiency.
Enhancing Accuracy and Reducing Errors
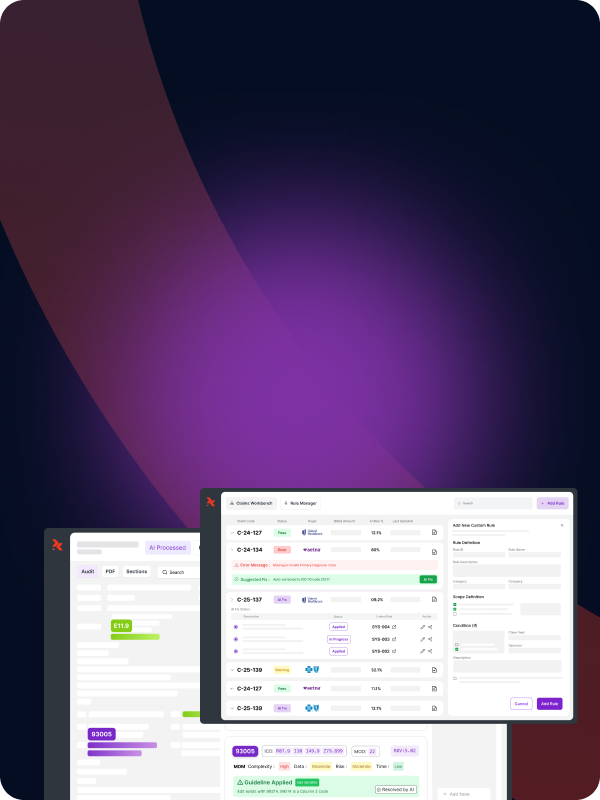
One of the most significant advantages of AI in medical coding is its ability to enhance accuracy. AI-powered coding systems, such as those developed by RapidClaims, utilize machine learning algorithms to analyze patient records, identify relevant codes, and ensure that all necessary codes are captured. This not only minimizes the risk of under-coding but also ensures that complex cases are accurately coded, leading to appropriate reimbursement.
AI systems can process vast amounts of data quickly, reducing the time it takes to code a patient’s record. By eliminating the need for manual coding, healthcare providers can significantly reduce the incidence of errors, such as missing modifiers or incorrect severity levels, which can result in denied claims or delayed payments.
Automating Routine Tasks
AI in medical coding also brings the benefit of automation, allowing healthcare providers to handle larger volumes of coding without increasing their workforce. Routine tasks, such as assigning ICD-10 codes or verifying patient eligibility, can be automated, freeing up coders to focus on more complex cases that require human oversight. This shift not only enhances team efficiency but also reduces labor costs and minimizes the need for additional coders as the organization scales.
Cost Savings and Scalability
As healthcare organizations continue to face financial pressures, the need for cost-effective solutions becomes more critical. AI-powered medical coding offers significant cost savings by reducing the reliance on human coders and minimizing the potential for costly errors. Furthermore, AI systems are scalable, meaning they can handle increased volumes of coding as the organization grows, without the need for proportional increases in staff.
Lowering Labor Costs
By automating routine coding tasks, AI systems reduce the need for a large coding workforce. This not only lowers labor costs but also allows healthcare organizations to allocate resources more effectively. Coders can be redeployed to supervisory roles, where they oversee AI-generated codes, or to other critical areas of the revenue cycle that require human intervention.
Additionally, AI systems are capable of processing codes 24/7, which means that coding backlogs can be cleared more quickly, and claims can be submitted faster. This leads to quicker reimbursements and improved cash flow, further enhancing the financial health of the organization.
Ensuring Compliance with Coding Standards
Compliance with coding standards is a key concern for healthcare providers, as errors or omissions can result in penalties or audits. AI systems, like those developed by RapidClaims, are designed to stay up-to-date with the latest coding standards and regulations. This ensures that all coding is compliant, reducing the risk of audits and the associated financial repercussions.
AI systems can also assist in training new coders by providing real-time feedback and suggestions. This not only helps to improve the accuracy of coding but also ensures that new coders are trained to the highest standards, further enhancing compliance.
Optimizing Revenue Cycle Management
The integration of AI into medical coding has a profound impact on revenue cycle management. By improving the accuracy and efficiency of coding, AI helps to optimize the entire revenue cycle, from patient intake to final payment. This leads to faster claims processing, fewer denied claims, and a more predictable cash flow.
Faster Claims Processing
With AI systems automating the coding process, claims can be generated and submitted to payers more quickly. This reduces the time it takes for healthcare providers to receive payment, improving cash flow and reducing the financial strain on the organization. Additionally, AI systems can track claims and flag any issues that may arise, ensuring that they are resolved promptly and do not delay payment.
Reducing Denied Claims
One of the main reasons for denied claims is coding errors. AI systems help to reduce the incidence of errors by ensuring that all necessary codes are captured and correctly applied. This not only improves the accuracy of coding but also reduces the likelihood of claims being denied. As a result, healthcare providers can expect to see a reduction in the number of denied claims and an increase in successful reimbursements.
Overcoming Challenges in AI Implementation
While the benefits of AI in medical coding are clear, healthcare organizations may face challenges in implementing these systems. These challenges include ensuring HIPAA compliance, managing different data formats, integrating AI systems with existing software, and addressing potential staff pushback.
Ensuring HIPAA Compliance
Medical coding systems that handle patient data must be secure and compliant with HIPAA regulations. AI systems must be designed with security in mind, ensuring that all patient data is protected and that the system is compliant with all relevant regulations. RapidClaims’ AI systems are built with these considerations at the forefront, ensuring that all coding and billing activities are conducted securely and in compliance with HIPAA standards.
Managing Data Formats and Integrations
Another challenge in implementing AI systems is managing different data formats and integrating the AI system with existing software. Healthcare organizations often use a variety of software systems, each with its own data formats. AI systems must be able to process data from these different sources and integrate seamlessly with existing software to ensure smooth operations.
RapidClaims’ AI systems are designed to be highly adaptable, capable of integrating with a wide range of software platforms. This ensures that healthcare providers can implement AI coding solutions without disrupting their existing workflows.
Addressing Staff Pushback
The introduction of AI systems may be met with resistance from staff, who may fear that their jobs are at risk. It is essential for healthcare organizations to communicate the benefits of AI to their staff and to emphasize that AI systems are designed to support, not replace, human coders. By involving staff in the implementation process and providing training on the new system, healthcare organizations can help to alleviate concerns and ensure a smooth transition to AI-powered coding.
The Future of AI in Medical Coding
The future of AI in medical coding is bright, with advancements in technology set to further revolutionize the healthcare industry. As AI systems continue to evolve, we can expect to see even greater improvements in accuracy, efficiency, and scalability.
AI-Powered Audits and Fraud Detection
One area where AI is likely to have a significant impact is in medical audits and fraud detection. AI systems can analyze vast amounts of data to identify patterns and anomalies that may indicate potential fraud or errors. This proactive approach could significantly reduce financial losses for healthcare providers and insurers, further enhancing the value of AI in medical coding.
Personalized Coding and Predictive Analytics
Another exciting development is the potential for AI to offer personalized coding based on a patient’s medical history, genetics, and current condition. This would allow for pre-emptive coding, streamlining billing processes and ensuring accurate reimbursement for complex or evolving cases. Predictive analytics could also be used to optimize revenue cycle management by identifying potential bottlenecks and addressing them before they become issues.
Conversational AI and Blockchain Integration
The integration of AI with other emerging technologies, such as conversational AI and blockchain, offers further opportunities for innovation. Conversational AI could be used to create virtual assistants that handle billing inquiries, schedule appointments, and manage insurance pre-approvals, freeing up human staff for more critical tasks. Blockchain integration could provide a secure and transparent billing ecosystem, enabling real-time claim validation and faster reimbursements.
Conclusion
AI is transforming the healthcare industry, particularly in the areas of medical coding and revenue cycle management. By enhancing accuracy, automating routine tasks, and optimizing the revenue cycle, AI systems are helping healthcare providers to improve their financial performance and deliver better patient care. While there are challenges to implementing AI, the benefits far outweigh the risks, making AI an essential tool for healthcare organizations looking to stay competitive in a rapidly evolving industry.
At RapidClaims, we are at the forefront of this transformation, offering AI-powered coding solutions that help healthcare providers streamline their operations, reduce costs, and improve compliance. As the future of AI in medical coding continues to unfold, we remain committed to delivering innovative solutions that meet the needs of healthcare providers and their patients.
%201.png)