.webp)
Unlocking the Future of Healthcare with AI-Driven Medical Coding

In the rapidly evolving landscape of healthcare, ensuring accuracy and efficiency in medical coding is more crucial than ever. Medical coding is the backbone of the healthcare revenue cycle, translating clinical documentation into standardized codes that are essential for billing, insurance claims, and overall patient care. However, the sheer volume and complexity of modern medical data present significant challenges, especially as the industry continues to grow at an impressive rate. Enter Artificial Intelligence (AI)—a transformative force that is reshaping how medical coding is approached, making the process faster, more accurate, and more compliant with regulatory standards.
The Growing Complexity of Medical Coding
The medical coding market is expected to grow at a compound annual growth rate (CAGR) of 8.0% from 2022 to 2030, according to Grand View Research. This growth is driven by an increasing volume of healthcare data, the majority of which is unstructured. Coders are often required to sift through free-text clinical notes, discharge summaries, test reports, and other intricate data stored in Electronic Health Records (EHRs) to find the correct codes. The latest ICD version alone consists of over 70,000 billing codes, making it a daunting task to ensure that each piece of clinical documentation is coded accurately.
The Impact of Coding Errors
Inaccurate medical coding can have far-reaching consequences, leading to increased claim denials, revenue losses, compliance risks, and ultimately, a negative impact on patient care. The Healthcare Financial Management Association (HFMA) reported that in 2021, approximately 90% of denied claims could have been avoided. These denials represent potential annual revenue losses of about $235 billion for the American medical industry.
With the healthcare industry undergoing a radical transformation towards a value-based care model, inaccurate coding not only hinders financial performance but also compromises the overall quality of care provided to patients.
The Rise of AI-Assisted Medical Coding
Traditional manual coding processes are becoming increasingly unsustainable in the face of growing data complexity. AI-driven medical coding solutions are emerging as a powerful tool to address these challenges, offering the potential to significantly improve both the speed and accuracy of the coding process.
How AI is Revolutionizing Medical Coding
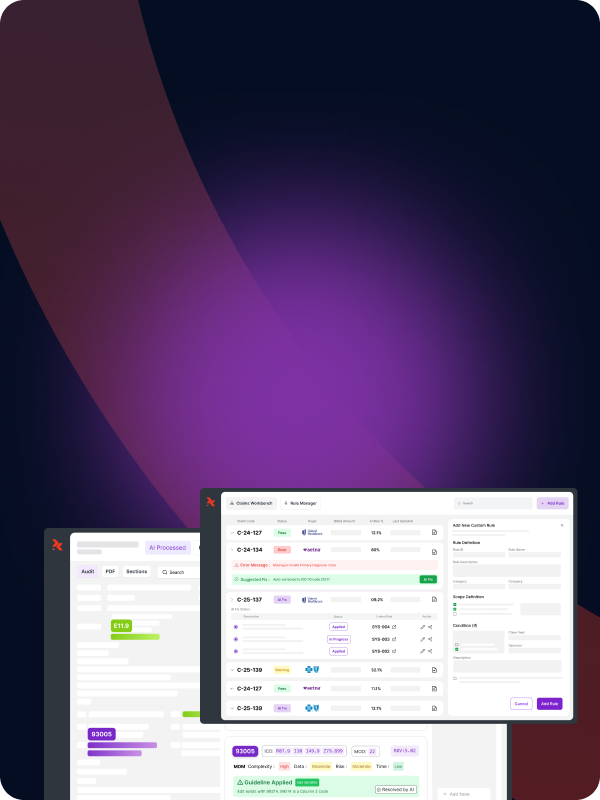
AI-assisted medical coding platforms leverage advanced technologies such as Natural Language Processing (NLP) and Machine Learning (ML) to automatically analyze and interpret medical data, mapping it to the appropriate codes with high precision. These platforms can process both structured and unstructured data, identify key medical phrases, and match them with the corresponding ICD codes, all while learning and improving over time.
By automating routine tasks, AI allows coders to focus on more complex and nuanced cases, thereby reducing the risk of errors and ensuring compliance with the latest coding standards. This not only enhances the accuracy of the coding process but also improves overall operational efficiency.
Real-World Application: AI in Action
Consider a Behavioral Wellness Center in Los Angeles that struggled with coding accuracy due to the unstructured nature of its EHR data, which included handwritten notes and various formats. The clinic faced frequent claim denials, leading to significant revenue losses and patient dissatisfaction.
By implementing an AI-assisted medical coding platform, the clinic was able to automatically extract and map the correct Z Codes to the relevant patient data, significantly improving coding accuracy and reducing claim denials. The platform's NLP capabilities allowed it to analyze and understand the context of medical documents, ensuring that the most appropriate codes were applied consistently and correctly.
Achieving the 3Cs of Medical Coding: Correctness, Consistency, and Compliance
AI-driven medical coding platforms are designed to excel in three critical areas that are essential for successful medical coding: correctness, consistency, and compliance.
1. Correctness
AI reduces the likelihood of human error by accurately interpreting complex medical documents and applying the correct codes. For example, when dealing with chronic diseases that present overlapping symptoms, AI can quickly and accurately identify the most appropriate code, reducing the time and effort required by human coders.
2. Consistency
NLP-powered AI platforms ensure consistency in coding by learning from previous cases and applying that knowledge to future coding tasks. This consistency is crucial for maintaining high standards of accuracy across all coding activities, particularly in large healthcare organizations where multiple coders may be involved.
3. Compliance
Compliance with healthcare regulations such as HIPAA is non-negotiable, and AI-enabled coding platforms are designed with this in mind. These platforms are regularly updated with the latest coding standards and guidelines, ensuring that all coding activities remain compliant with current regulations. Additionally, AI can flag potential compliance issues, allowing organizations to address them before they lead to costly penalties or legal actions.
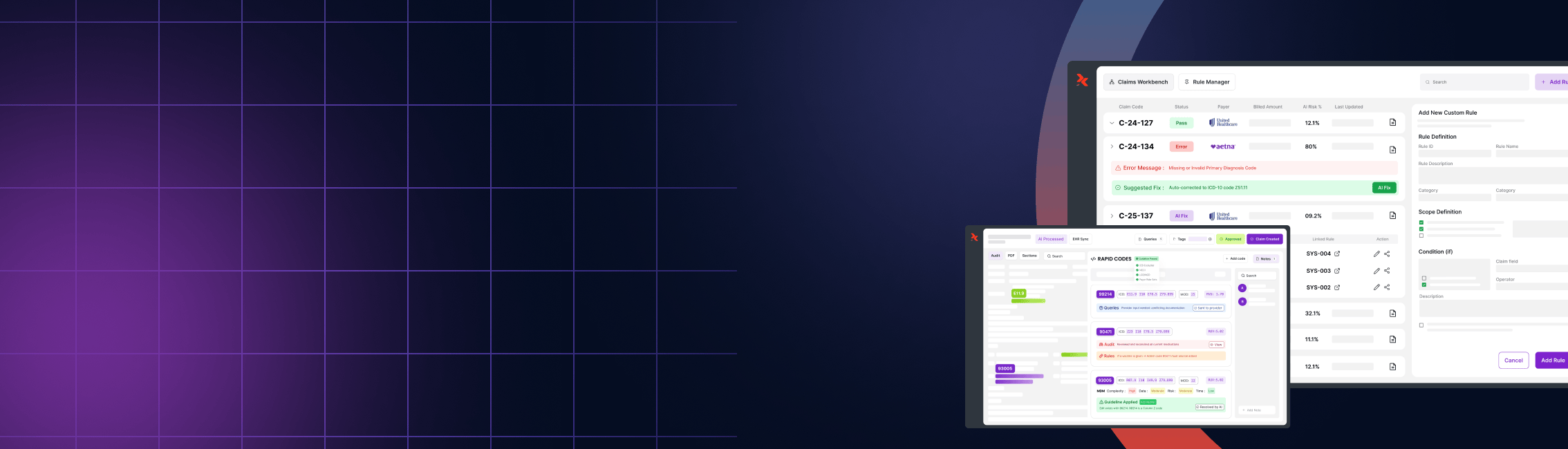
The Role of RapidClaims in the AI Revolution
As a leader in AI-driven medical coding solutions, RapidClaims is at the forefront of this transformation. Our platform is designed to streamline the coding process, enhance accuracy, and ensure compliance, all while reducing costs and improving operational efficiency. By automating routine coding tasks, we empower healthcare organizations to scale their operations without the need for additional coders, making it easier to handle large volumes of data.
Process Improvement
At RapidClaims, we are committed to process improvement through the use of the latest AI technologies. Our platform integrates seamlessly with existing EHR systems, allowing for real-time data analysis and code generation. This integration not only speeds up the coding process but also ensures that all codes are applied correctly and consistently.
Team Efficiency
One of the key benefits of our AI-driven platform is the reduction in manual coding tasks, which allows healthcare teams to focus on more complex and value-added activities. This leads to higher productivity and job satisfaction among coders, as well as better outcomes for patients.
Cost Savings
By automating the most time-consuming aspects of medical coding, RapidClaims helps healthcare organizations significantly reduce their labor costs. Additionally, the increased accuracy provided by our platform minimizes the risk of claim denials, resulting in faster reimbursements and improved cash flow.
Accuracy Enhancement
Our platform's AI algorithms are constantly learning and improving, ensuring that the highest levels of accuracy are maintained across all coding activities. This is particularly important in complex cases where precise coding is critical to ensuring that patients receive the appropriate care and that healthcare providers are reimbursed correctly.
Compliance Assurance
RapidClaims is fully committed to compliance with all relevant healthcare regulations. Our platform is regularly updated with the latest coding standards and guidelines, and it includes built-in tools to identify and address potential compliance issues.
Technical Scalability
As healthcare organizations grow and take on more patients, the ability to scale coding operations becomes increasingly important. RapidClaims is designed to handle large volumes of data with ease, making it the ideal solution for organizations looking to expand their operations without compromising on accuracy or efficiency.
Optimization
At the heart of our platform is a commitment to optimization—whether it’s optimizing the coding process, improving team efficiency, or enhancing overall operational performance. By providing healthcare organizations with the tools they need to succeed, RapidClaims is helping to shape the future of medical coding.
Moving Forward with AI-Driven Medical Coding
The adoption of AI-driven medical coding platforms is no longer a luxury but a necessity for healthcare organizations looking to stay competitive in today's fast-paced environment. By leveraging the power of AI, these organizations can overcome the challenges associated with traditional coding processes, improve their revenue cycle management, and ultimately provide better care to their patients.
As the medical coding industry continues to evolve, RapidClaims remains dedicated to leading the way with innovative solutions that drive accuracy, efficiency, and compliance. Whether you are a small clinic or a large healthcare system, our platform is designed to meet your needs and help you achieve your goals.
In conclusion, the future of medical coding lies in the hands of AI. With the right tools and technologies, healthcare organizations can not only overcome the challenges of today but also prepare for the opportunities of tomorrow. At RapidClaims, we are proud to be a part of this exciting journey, and we look forward to continuing to serve our clients with the best in AI-driven medical coding solutions.
For more information on how RapidClaims can help transform your medical coding processes, visit our website or contact us today.
Key Takeaways:
- The complexity of medical coding is increasing, with over 70,000 ICD codes to navigate.
- AI-driven platforms like RapidClaims are revolutionizing the medical coding process, improving accuracy, consistency, and compliance.
- By automating routine tasks, AI allows healthcare teams to focus on more complex cases and reduces the risk of coding errors.
- RapidClaims is committed to helping healthcare organizations improve their revenue cycle management through innovative AI solutions.
%201.png)